How to Write a SOAP Note: 7 Tips to Get Started
Best Practices for Writing High-Quality, Efficient SOAP Notes
Key Takeaways
- Knowing how to write a SOAP note (Subjective, Objective, Assessment, Plan) is essential for documenting patient interactions effectively.
- Good documentation is crucial for saving time and reducing errors in patient care.
- Best practices for notetaking include consistency, avoiding jargon for clarity, and verifying information regularly.
- Accurate and detailed clinical notes aid in better clinical decision-making.
- IntakeQ streamlines the documentation process, making it faster and more precise.
Accurate and efficient SOAP notes are the backbone of quality healthcare.
But imagine trying to piece together a patient’s history from scattered, incoherent notes. It’s like piecing together a story with important chapters missing.
That’s why learning how to write a good SOAP note is vital. It can help you get the full story so you can better understand your patient and provide quality care.
Whether you’re a seasoned clinician refining your skills or a newcomer eager to learn, a good notetaking strategy can elevate your practice and improve patient care. Here’s what you need to know:
What is a SOAP Note?
SOAP stands for Subjective, Objective, Assessment, and Plan. Each section gives a detailed snapshot of a patient’s condition and treatment plan. This format ensures that nothing gets missed and everyone on the care team is on the same page. By breaking things down into these four parts, these notes can help you and your team deliver well-coordinated and efficient care.
Why Treatment Notes Are Vital in Healthcare
Clinical notes ensure clear and precise communication among healthcare providers. Imagine a patient with diabetes being referred from their primary care physician to an endocrinologist. Without detailed treatment notes capturing their symptoms, medication history, and lab results, essential information might be overlooked. Well-documented notes ensure every specialist has a complete picture, promoting seamless continuity of care.
Beyond communication, your notes play a vital role in making informed clinical decisions and providing a robust legal record of patient interactions. For example, if a patient’s treatment plan is ever questioned, detailed documentation can demonstrate the rationale behind each decision, protecting healthcare providers. By using them, you not only improve patient care but also safeguard your practice with documented evidence of the treatments and decisions made.
Breaking Down the S-O-A-P
Subjective: The Patient’s Perspective
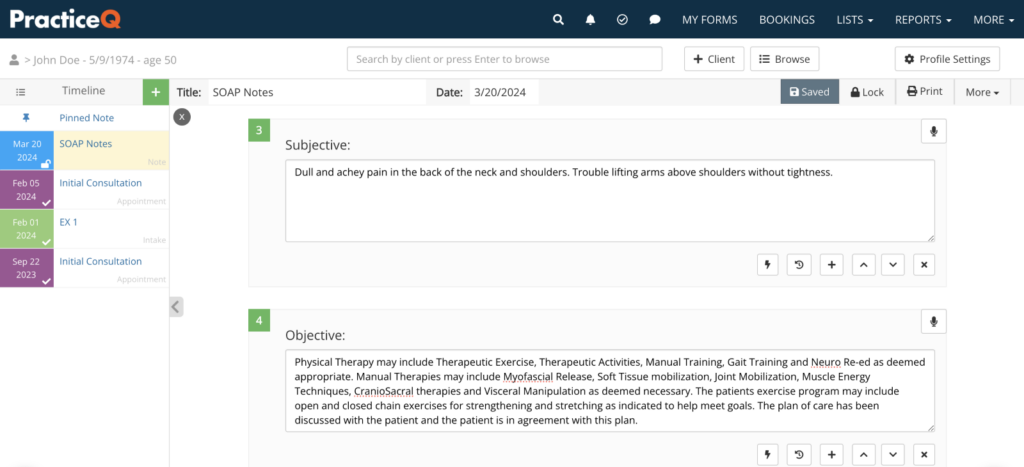
The Subjective section captures the patient’s own words about their condition, including symptoms, concerns, and feelings. For example, a patient might describe their pain as “sharp and stabbing” or mention feeling dizzy. These personal insights are important as they provide context and help in tailoring the care plan to their specific experiences.
Objective: Measurable Data
The Objective section includes measurable data and observations that validate the patient’s subjective complaints. This can encompass vital signs like blood pressure and heart rate, as well as lab results and physical exam findings.
Assessment: Clinical Evaluation
In the Assessment section, the clinician synthesizes the subjective and objective data to form a diagnosis. It involves clinical judgment and may include differential diagnoses—essentially a list of potential conditions that could be causing the patient’s symptoms.
Plan: Treatment Strategy
The Plan section outlines the next steps in the patient’s care, providing a clear roadmap for treatment. This can include prescribed medications, recommended tests, follow-up appointments, and lifestyle changes.
7 Best Practices for Writing High-Quality SOAP Notes
1. Be Clear and Concise
Use simple, clear language. Avoid unnecessary jargon to ensure anyone can read your notes.
2. Use Standardized Terminology
While you should avoid being overly complex, still take care to use standardized medical terms. It maintains consistency and helps prevent misunderstandings among healthcare providers.
3. Prioritize Relevant Information
Focus on information directly relevant to the patient’s condition and treatment. Avoid extraneous details.
4. Organize Your Thoughts Logically
Tell your patient’s story. Ensure that each section of the treatment note flows logically from one to the next, providing a coherent narrative of the patient’s visit.
5. Document Patient’s Subjective Input Thoroughly
Patient feedback plays a significant role in accurate diagnosis and treatment. Capture every symptom and concern in detail.
6. Update Notes Promptly
Always update your notes to reflect any changes in the patient’s condition or treatment plan.
7. Review and Revise
Lastly, take a moment to review your notes for accuracy and completeness before finalizing them. This way, you can catch any errors or add information that may have been left out.
How to Use Technology for Better, Faster SOAP Notes
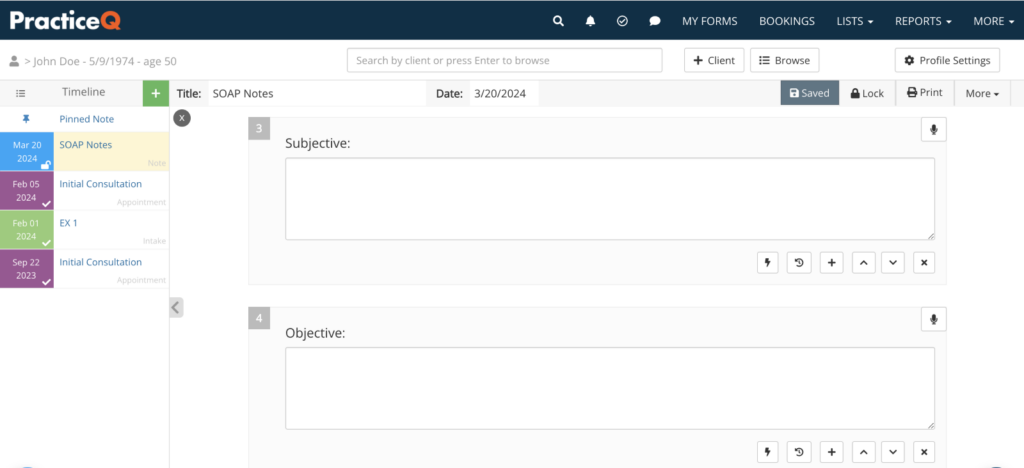
Healthcare documentation can be tedious, but technology can simplify the process. IntakeQ provides customizable templates that fit your needs—whether it’s text fields, diagrams, or attachments.
IntakeQ automates healthcare documentation through several key features:
- Pre-filled templates. Start with standardized templates tailored to your practice, which you can customize as needed.
- Auto-population. Relevant patient information is auto-populated from their records, saving time on repetitive data entry.
- Voice-to-text. Use voice recognition to dictate your notes directly into the system.
- Quick access buttons. Easily insert common phrases or data points with a single click.
The Benefits of IntakeQ’s Treatment Notes
With IntakeQ’s automation, customization, and easy-to-use dashboard, you gain several benefits that streamline your documentation process:
- Keep all your clinical notes in one place, making it simple to stay organized and quickly find what you need.
- Standardized templates ensure your documentation is always clear and accurate, reducing the chance of miscommunication.
- With IntakeQ’s secure online portal, you can easily update and communicate with patients, ensuring timely updates and better care continuity.
- Automating your notes saves time and boosts productivity, letting you focus more on your patients.
The Bottom Line
Good documentation is essential to the care you provide. With clear, accurate SOAP notes, you can capture every detail of patient interactions, enabling better communication and continuity of care. They also save valuable time, reduce errors, and improve the overall quality of your practice.
And with IntakeQ, you can streamline your treatment notes effortlessly, simplifying the process so you can focus on superior patient care.
See how effortless clinical note automation can improve your practice. Try IntakeQ free for 14 days and see how automation can transform your patient care.
SOAP Note FAQs
What are SOAP notes and why are they important?
SOAP notes (Subjective, Objective, Assessment, Plan) are a structured method for documenting patient interactions in healthcare. They provide a consistent format that helps ensure comprehensive and clear documentation of patient care.
How do SOAP notes improve communication among healthcare providers?
By following a standardized format, treatment notes make it easier for different healthcare providers to understand and follow a patient’s history and treatment plan, facilitating better teamwork and continuity of care.
What common mistakes should be avoided when writing treatment notes?
It’s important to avoid using ambiguous language and medical jargon, not updating the notes promptly, and missing out on key details that could be critical for patient care.
How can IntakeQ support healthcare providers in managing clinical notes?
IntakeQ helps healthcare providers by automating the treatment note process, making it faster and more accurate, and reducing the administrative burden so they can focus more on patient care.
Can my treatment notes be integrated with electronic health records (EHR)?
Yes, your notes can often be integrated with electronic health records (EHR) systems, allowing for seamless documentation and easy access to patient information across different platforms and by various healthcare providers.
References
Lew, V., Ghassemzadeh, S., & Podder, V. (2023, August 28). SOAP Notes. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482263/
Purdue Writing Lab. (2018). SOAP Notes. Purdue Writing Lab. https://owl.purdue.edu/owl/subject_specific_writing/healthcare_writing/soap_notes/index.html

