How to Write Impactful Therapy Progress Notes (with Examples)
The Therapist’s Handbook for Effective Documentation That Makes a Difference
Key Takeaways
- Therapy progress notes are essential for tracking client progress and ensuring continuity of care.
- Compliant notes protect your practice legally and support accurate billing.
- Well-structured notes improve client sessions and improve collaboration with other healthcare providers.
- Different frameworks like SOAP, DAP, and BIRP notes can streamline your documentation process.
- IntakeQ offers tools to make your therapy documentation more efficient and effective.
Have you ever found yourself staring at a blank screen, unsure of how to capture the essence of a therapy session in your progress notes? You’re not alone.
Writing effective and compliant therapy progress notes is a challenge many therapists face. However, it’s crucial for providing quality care and maintaining thorough documentation.
Here, we’ll explore the best practices for creating compliant and effective therapy notes so you can make the biggest impact in your clients’ therapeutic journeys.

What Are Therapy Progress Notes?
Therapy progress notes go beyond simply recording what happened during a session. These notes serve as a detailed account of the client’s progress towards treatment goals, helping to ensure continuity of care and providing a clear narrative of the client’s therapeutic journey.
Unlike psychotherapy notes, which are private and generally not shared, progress notes are designed to be shared with other healthcare providers, insurance companies, and legal entities when necessary.
A well-structured progress note should answer key questions:
- How did the client present during the session?
- What interventions were used?
- How did the client respond to those interventions?
The Importance of Writing Compliant Notes
Writing compliant progress notes is essential for maintaining the quality and legality of your practice. Compliance ensures that your notes meet the ethical, professional, and regulatory standards required in therapy. This includes adhering to guidelines set by your licensing board, meeting insurance documentation requirements, and ensuring that your notes are clear and thorough for sharing with other healthcare providers when needed.
Compliant notes protect your practice legally, support your billing claims, and provide an accurate record of the client’s progress. Additionally, they facilitate collaboration, as they’re intended to be shared and reviewed by other healthcare professionals involved in the client’s care.
Benefits of Well-Written Progress Notes
Beyond compliance, well-written progress notes offer several key benefits that enhance your therapeutic practice:
Improve Client Therapy Sessions
Good notes improve your ability to recall details between sessions, helping avoid repetition of ineffective interventions. Plus, they demonstrate your attentiveness and commitment to the client’s progress.

Protect Your Practice
Thorough documentation can protect you in legal situations by providing a clear record of the care provided. This is especially important in cases where the client’s history needs to be reviewed by other healthcare providers or in legal proceedings.
Strengthen Team Collaboration
Detailed progress notes make it easier for other healthcare providers involved in the client’s care to understand their history and current treatment, ensuring a cohesive approach.
How to Structure Your Therapy Documentation
Structured therapy documentation is key to ensuring clarity, consistency, and compliance in your progress notes. Importantly, it helps you include all necessary details to create a comprehensive record that supports both therapeutic outcomes and legal requirements.
Let’s break down what you should include in every note:
1. Session Overview
Start with a concise record of the session specifics:
- Date, time, and setting
- Whether it’s in-person or virtual
- Client information
- Your name and credentials
2. The Client’s Story
Capture the essence of the client’s experience by highlighting their own words and emotional tone:
- Reflect the client’s perspective
- Provide insights into their mental and emotional state
- Support personalized care
3. Clinical Observations
Document your professional insights into the client’s current mental health status:
- Behavior and appearance
- Emotional state
- Cognitive processes
4. Goal Tracking
Assess the client’s progress towards their therapeutic goals:
- Observe any strides made
- Note challenges faced or areas of plateau
- Evaluate treatment effectiveness
5. Safety and Risk Evaluation
Conduct a comprehensive review of any potential risks:
- Identify risks like self-harm or threats
- Outline discussed safety measures
- Reinforce ethical standards and duty of care
6. What’s Next
Finally, you should focus on the next steps in the client’s therapeutic journey:
- Detail techniques or exercises for future sessions
- Suggest activities for client progress
- Provide a clear, actionable path forward
These are your foundational elements—the content that forms the backbone of effective progress notes. But when it comes to putting it all together, a structured framework can be helpful.
Here are three common types you can use to get started: SOAP notes, BIRP notes, and DAP notes.
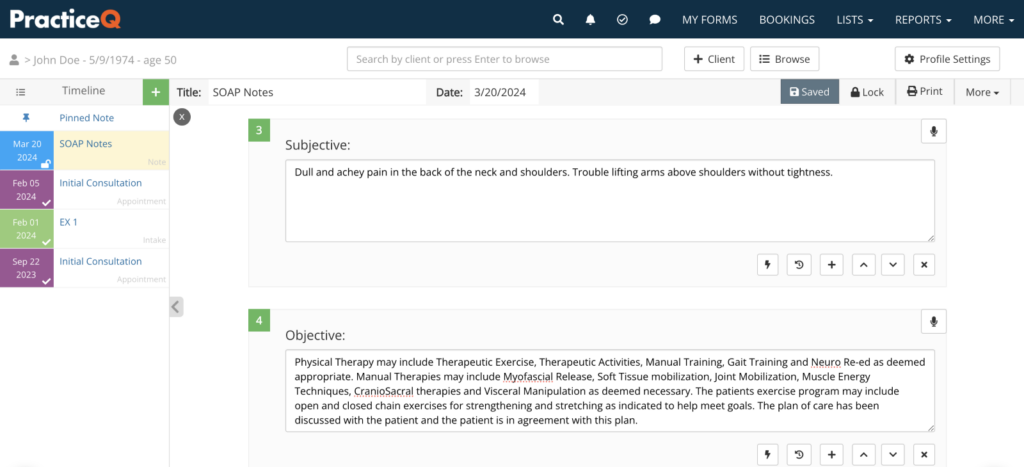
SOAP Notes (Subjective, Objective, Assessment, Plan)
- Subjective: Capture the client’s narrative, focusing on their personal experiences, emotions, and any reported symptoms.
- Objective: Document factual observations, including the client’s appearance, behavior, and other measurable data.
- Assessment: Provide a professional evaluation of the client’s condition, integrating subjective and objective information to form a clinical impression.
- Plan: Outline the proposed treatment steps, including interventions and therapeutic goals, to guide future sessions.
Altogether, SOAP notes offer a comprehensive framework that balances personal insights with clinical objectivity. This makes them ideal for detailed session analysis.
SOAP Notes Example
| Client Name: Gregory Johns Date of Birth: 07/15/1985 Date of Service: 10/15/2023 Session Location: In-person, office setting Start and End Time: 2:00 pm – 2:50 pm Subjective: Alex reports feeling “anxious and overwhelmed” due to increased workload at his job and recent family commitments. He describes difficulty concentrating at work and experiencing tension headaches. Alex mentions that his sleep has been disrupted, often waking up in the middle of the night with racing thoughts. He expresses concern about his ability to manage stress and is seeking strategies to cope effectively. Objective: Alex appeared tense, with a furrowed brow and fidgeting hands throughout the session. His speech was rapid and pressured, indicating heightened anxiety. He maintained appropriate eye contact and was cooperative during the session. Alex’s mood was anxious, and his affect was congruent with his reported stress levels. Assessment: Alex is experiencing symptoms consistent with generalized anxiety disorder, exacerbated by recent life stressors. His anxiety is impacting his daily functioning, particularly in his professional and personal life. Alex demonstrates insight into his condition and is motivated to develop coping mechanisms to manage his anxiety effectively. Plan: Introduce Alex to mindfulness techniques to help manage immediate stress responses. Begin cognitive-behavioral therapy (CBT) to address negative thought patterns contributing to his anxiety. Encourage Alex to establish a regular sleep routine to improve sleep quality. Schedule a follow-up session in one week to evaluate progress and adjust the intervention plan as necessary. |
DAP Notes (Data, Assessment, Plan)
- Data: Consolidate both subjective experiences and objective findings into a cohesive overview of the session.
- Assessment: Analyze the gathered data to interpret the client’s current state and progress, drawing on clinical expertise.
- Plan: Detail actionable steps and recommendations for continuing treatment, focusing on addressing identified issues.
DAP notes simplify the documentation process by merging subjective and objective elements, providing a streamlined yet thorough record.
BIRP Notes (Behavior, Intervention, Response, Plan)
- Behavior: Note specific behaviors exhibited by the client, alongside their verbal expressions and mood.
- Intervention: Record the therapeutic techniques and interventions applied during the session.
- Response: Evaluate the client’s reaction to the interventions, noting any changes or progress observed.
- Plan: Develop a strategic plan for upcoming sessions, aimed at building on successes and addressing ongoing challenges.
Unlike SOAP and DAP notes, BIRP notes specifically highlight the interventions and client responses, making them particularly useful for tracking therapeutic progress.
Choosing the Right Framework for Your Practice
Each of these templates offers practical benefits tailored to different aspects of therapy, helping you capture important details and streamline your workflow. By selecting the framework that best suits your practice, you can improve the quality of care you deliver and support better outcomes for your clients.
Consider starting with the template that aligns most closely with your current needs, and gradually integrate it into your sessions. Furthermore, seek feedback from peers or supervisors to refine your approach, and don’t hesitate to adapt the templates to better fit your unique style and client needs.
Transform Your Therapy Documentation with IntakeQ
Effective notetaking is a fundamental aspect of delivering high-quality therapy. It provides a structured way to track client progress and enhance continuity of care. And as therapy practices evolve, digital tools have become essential to optimize these processes and focus on patient care.
IntakeQ, a digital forms solution, offers a user-friendly platform to make documentation seamless and efficient. Here’s how IntakeQ can support your work:
- Dynamic Note Templates: Create customizable templates using a variety of question formats, including diagrams and file attachments.
- Comprehensive Client Timeline: Access and manage treatment notes, intake forms, and appointments all from one place, ensuring a holistic view of client interactions.
- Efficient Note Snippets: Save time with reusable note snippets, allowing quick customization for each client’s unique needs.
- All-in-One Management: From online intake forms to secure patient portals, IntakeQ consolidates your practice management tasks, improving patient interactions and operational efficiency.
With IntakeQ, transforming your therapy documentation is just the beginning. Elevate your practice and client care effortlessly. Start your free 14-day trial today and experience the difference.
Therapy Documentation FAQS
How can I ensure my notes are both thorough and time-efficient?
Therapists often struggle to balance detailed documentation with time constraints. It’s important to develop a consistent note-taking routine that captures essential client information while being mindful of time. Using templates tailored to your practice can help streamline the process without sacrificing the quality of your notes.
What are the risks of poor documentation, and how I prevent them?
Inadequate documentation can lead to legal risks, ethical issues, and challenges in client care continuity. To mitigate these risks, therapists should ensure their notes are accurate, comprehensive, and in line with professional guidelines. Moreover, regular audits of your documentation practices can help identify and correct potential issues before they escalate.
How do I know if my practice needs to upgrade to a digital documentation platform?
If you find it challenging to keep your documentation organized, secure, and accessible, or if you spend too much time on paperwork, it’s time to consider a digital solution. A digital platform can streamline your workflow, improve efficiency, and help you stay compliant with evolving industry standards.
How can I improve the quality of my documentation to better support client outcomes?
High-quality documentation is key to effective therapy. Regularly reviewing and refining your documentation practices, seeking feedback from peers, and staying updated on best practices in the field can enhance the quality of your notes. Likewise, consider continuing education on documentation to ensure that your practices support optimal client outcomes.
Why should I consider using a digital platform like IntakeQ for my documentation?
IntakeQ streamlines your documentation by offering customizable templates, seamless integration with your practice tools, and secure, HIPAA-compliant features—all designed to save you time and keep your focus on client care.
References
Ludwick, M. (2023, September 12). Psychotherapy Notes and Progress Notes: What’s the Difference? | The Cooperative of American Physicians. Cooperative of American Physicians. https://www.capphysicians.com/articles/psychotherapy-notes-and-progress-notes-whats-difference
Norton, C. (2024, July 17). How to Write a SOAP Note: 7 Tips to Get Started. IntakeQ. https://blog.intakeq.com/how-to-write-a-soap-note-7-best-practices/
Stevens, K. (2024, May 2). How to Write DAP Notes in Private Practice: A Therapist’s Guide. The Private Practice pro | Kelley Stevens, LMFT. https://theprivatepracticepro.com/write-dap-notes-private-therapy-practice/

